Towards a treatment of erythropoietic protoporphyria
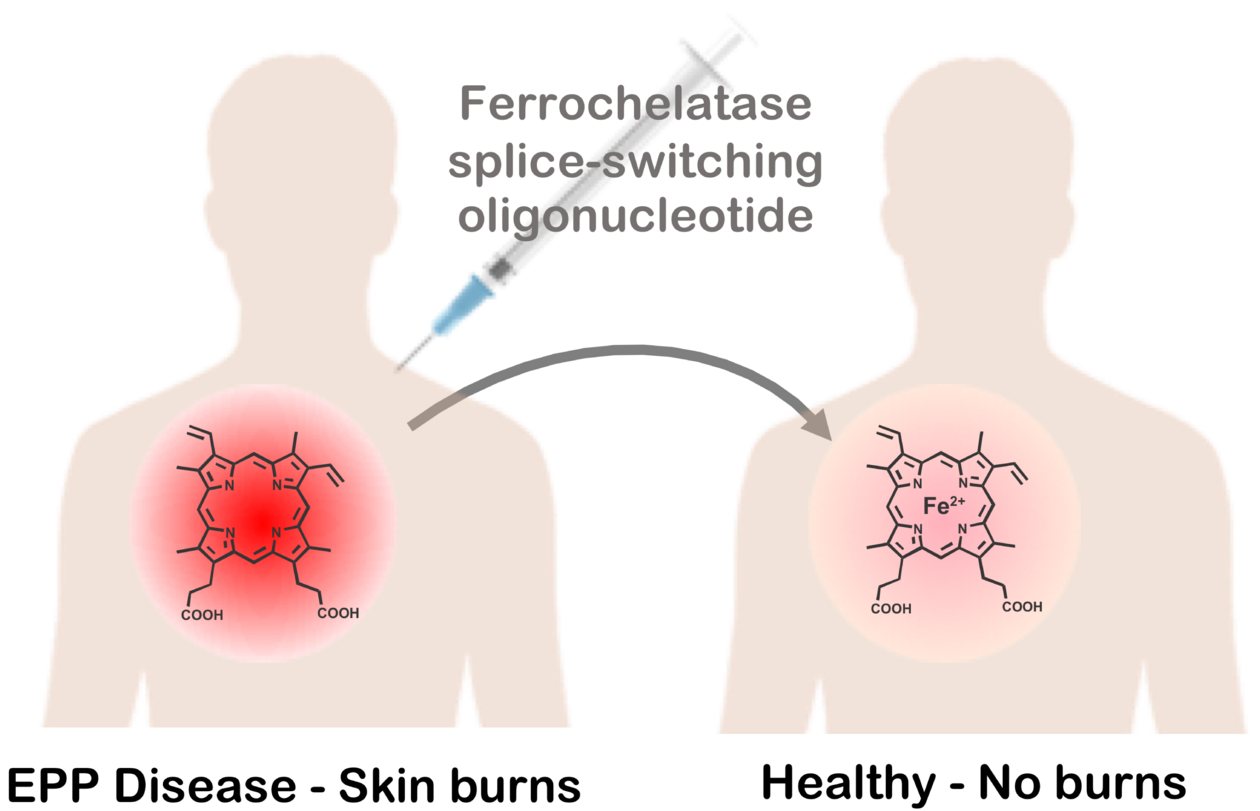
Erythropoietic protoporphyria (EPP) is a rare genetic disease, in which patients suffer burn-like injuries of the skin and severe pain after exposure to sunlight. A subgroup of patients will go on to develop hepatic complications with the risk of liver failure. EPP is caused by a deficiency in the enzyme ferrochelatase (FECH), which catalyses the insertion of iron into protoporphyrin IX (PPIX) to generate haem. This results in PPIX accumulation in red blood cells. Upon exposure to light, PPIX produces reactive oxygen species that trigger lipid peroxidation, cell membrane damage and inflammation.
In nearly all patients, one FECH allele contains a deleterious mutation whilst the other carries a T>C single nucleotide polymorphism in the third intron. This polymorphism causes the usage of an alternative splice site, yielding an mRNA that harbours a premature termination codon. Consequently, the mRNA is degraded by a nonsense mediated decay mechanism, resulting in reduced levels of FECH protein and activity.
A research team from ETH Zurich and the University of Bern, in collaboration with clinical researchers and patients from the Triemli Hospital and the University Hospital Zurich has now published a study in Nucleic Acids Research, in which they describe the development of a potent splice-switching oligonucleotide (SSO) that serves as a proof-of-concept for a future new treatment for EPP. “The management of the EPP condition largely relies on avoiding exposure to sun, severely impacting patients' quality of life. There is an urge to develop a therapeutic strategy that directly addresses the pathological mechanism”, Jonathan Hall, one of the corresponding authors of the study, explains.
The application of oligonucleotides represents a promising strategy for EPP, especially given their recent success employed to treat other genetic diseases, such as spinal muscular atrophy. SSOs are a class of antisense oligonucleotide that modify the splicing of pre-mRNA to which they hybridize with high affinity and selectively in the cell nucleus. This creates a "steric block" to the binding of alternative splicing factors, thereby altering the outcome of splicing. Since the splicing-altering T>C polymorphism is present in nearly all EPP patients, a single SSO could provide therapeutic benefit to almost the entire EPP patient population.
Using a FECH reporter system in cells, the authors identified one SSO from a small library of oligonucleotides that binds to the T>C polymorphism and reverses the splicing defect. To generate an SSO that is effective in vivo, the team conjugated the oligonucleotide to different chemical groups that were expected to increase its stability and the delivery to selected tissues. They administered the conjugated SSOs to a first generation EPP mouse model and studied its distribution, its metabolic stability and, most importantly, its splice-switching ability at the FECH locus in different organs.
Jonathan Hall explains that one of the main challenges for the development of an SSO to treat EPP is its delivery to erythroblasts in the bone marrow, the organ in which the great majority of PPIX is synthesized. “We really didn’t know whether there would be any effect in vivo at all, since historical data from the literature has shown that SSOs in the bone marrow were ineffective.” Remarkably, the authors demonstrated that an SSO conjugated to cholesterol group boosts the levels of the correctly-spliced FECH transcript by 80% in the bone marrow of EPP mice.
Future work will aim to further improve cholesterol-conjugated SSOs, so as to maximize their stability for systemic delivery and potentially further increase their splicing-correction. In parallel with these efforts, the team is currently working on a new EPP mouse model to help determine whether these FECH SSOs can alleviate the painful skin lesions suffered by EPP patients. The development of an SSO delivery strategy to the bone marrow is not only a promising treatment for EPP but also for other diseases that arise from splicing deficiencies manifested in cells of the bone marrow.
Halloy et al. (2020) NAR, 48(9):4658-4671 (Open Access)
Text: Veronika Herzog